Now Reading: Yaşlı Nazofarengeal Kanser Hastalarında İmmünoterapinin Faydaları ve Riskleri
-
01
Yaşlı Nazofarengeal Kanser Hastalarında İmmünoterapinin Faydaları ve Riskleri

Yaşlı Nazofarengeal Kanser Hastalarında İmmünoterapinin Faydaları ve Riskleri
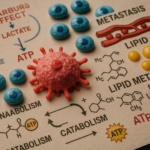
Elderly patients suffering from recurrent or metastatic nasopharyngeal carcinoma (RM-NPC) have long faced unique challenges in cancer treatment. The advent of immunotherapy, particularly immune checkpoint inhibitors (ICIs), marks a significant turning point in oncological care for this demographic. Recent findings from a noteworthy study published in BMC Cancer indicate that immunotherapy could reshape the treatment approaches for elderly individuals battling RM-NPC. This study specifically focuses on patients aged 65 and older, addressing a crucial gap in the clinical understanding of this vulnerable population.
Nasopharyngeal carcinoma, especially prevalent in southern China and Southeast Asia, presents distinct medical challenges when it recurs or metastasizes. Traditionally, patients with RM-NPC have undergone a combination of chemotherapy and ICIs. Yet, older adults often carry additional health concerns that complicate their response to treatment. This study’s retrospective analysis of 95 elderly RM-NPC patients, treated between January 2015 and February 2022, sought to illuminate how the elderly fare in terms of safety and effectiveness when treated with these innovative therapies.
A notable aspect of the study was its rigorous methodology. Utilizing advanced statistical models, including Cox regression, researchers were able to assess survival outcomes meticulously. The patients included in this study primarily comprised males, and their evaluations were supported by comprehensive geriatric assessments that employed well-established comorbidity indices like the ACE-27 and the Charlson Comorbidity Index (CCI). This attention to detail allowed for a nuanced understanding of the interplay between existing health conditions and treatment outcomes.
One of the study’s striking findings was the increased benefit associated with the addition of local therapy—such as targeted radiation or ablative procedures—when combined with systemic immunotherapy. A hazard ratio of 0.352 indicated a nearly two-thirds reduction in the risk of disease progression. This emphasizes the critical nature of a multimodal approach to treatment in elderly patients, suggesting that localized interventions can meaningfully improve progression-free survival even in advanced stages of cancer.
It’s also significant that this research found no considerable differences in survival rates or toxicity profiles among various age groups within the elderly cohort or among different types of ICIs used, challenging prior assumptions that older patients might suffer disproportionately from adverse treatment effects. This not only underscores the efficacy of immunotherapy in elderly patients with RM-NPC but also allays fears regarding their ability to tolerate such aggressive treatment regimens.
The median follow-up period of approximately two and a half years provided robust longitudinal insights, highlighting the sustained effectiveness and safety of immunotherapy for this age group. Continuous monitoring during this period did not reveal unexpected toxicity signals, further reinforcing the applicability of these findings to broader clinical practice. Long-term data are integral to understanding the longevity of treatment benefits and managing potential delayed adverse events.
Moreover, the study shines a light on the systemic underrepresentation of older adults in clinical trials, a phenomenon that has limited the generalizability of many oncological findings. By centering the research specifically on geriatric patients, the authors have sought to provide crucial evidence that can guide oncologists in making informed decisions regarding immunotherapy for older patients, previously circumscribed by a lack of robust data.
The innovative use of comorbidity scoring systems in the study enhances its credibility. By evaluating patients’ overall health status—incorporating non-cancer-related conditions—the research offers insights into how these factors can influence treatment outcomes separately from tumor biology. This methodology aids healthcare providers in identifying which elderly patients might be most amenable to aggressive therapeutic approaches, fostering a more personalized treatment framework.
As immunotherapy continues to evolve, the study also highlights the importance of developing tailored treatment plans for elderly patients based on individual cancer characteristics and overall health. The absence of significant variations among different ICI agents suggests that clinicians may have flexibility in selecting drugs based on availability and patient tolerance, thereby expanding the range of therapeutic options available.
The findings of this comprehensive study invite further investigation into combination therapeutic regimens that might integrate local treatments with systemic ICIs. As treatments advance, the potential for optimizing patient outcomes by blending immunotherapy with other modalities like radiation, localized chemotherapy, or ablative therapies is worth exploring, especially for those with complex clinical presentations.
Additionally, the implications of this research extend beyond oncology, sparking interest in studying immune system function in aging populations at large. The apparent effectiveness of immunotherapy challenges preconceived notions about the diminished capabilities of aging immune systems, opening avenues for exploring immunologically driven treatments for various diseases among older adults.
In summary, the findings from this pivotal study published in BMC Cancer compel the oncology community to rethink the current frameworks of immunotherapy application. Advancing age should not serve as an exclusion criterion for innovative cancer treatments. The study emphasizes the importance of multimodal interventions and strengthens the argument for the tolerability and efficacy of ICIs among elderly patients suffering from RM-NPC. These insights pave the way for more personalized, effective, and hopeful cancer care strategies that stand to significantly improve survival and quality of life in a demographic that has been historically underserved in cancer research.
As the oncology landscape continues to evolve, it is essential that clinical practices adapt to incorporate robust geriatric evaluations, ensuring that elderly patients receive the advanced treatments they need. This study lays a solid foundation for subsequent clinical trials and real-world applications that could revolutionize outcomes for older individuals facing the challenges posed by recurrent or metastatic nasopharyngeal carcinoma.
Araştırma Konusu: Elderly patients (≥65 years) with recurrent or metastatic nasopharyngeal carcinoma and the efficacy and safety of immunotherapy treatment.
Makale Başlığı: Effect and safety of immunotherapy among elder patients (age ≥ 65) with recurrent or metastatic nasopharyngeal carcinoma.
Haberin Yayın Tarihi: 2025.
Web References: https://doi.org/10.1186/s12885-025-14108-w
Doi Referans: https://doi.org/10.1186/s12885-025-14108-w.
Resim Credits: Scienmag.com.
Anahtar Kelimeler: immunotherapy, elderly patients, nasopharyngeal carcinoma, immune checkpoint inhibitors, cancer treatment, geriatric assessments, multimodal treatment approaches, clinical research, survival outcomes, comorbidities, advanced cancer therapies.