Now Reading: Pemetreksed, Platin ± Pembrolizumab Kombinasyonunun Güvenlik Profili
-
01
Pemetreksed, Platin ± Pembrolizumab Kombinasyonunun Güvenlik Profili
Pemetreksed, Platin ± Pembrolizumab Kombinasyonunun Güvenlik Profili
Lung cancer remains a pivotal challenge in global oncology, ranking as one of the foremost causes of cancer-related deaths worldwide. Historically, the combination of platinum-based chemotherapy with pemetrexed has been a standard therapeutic approach offering modest survival benefits. However, recent advancements in immunotherapy have notably transformed treatment paradigms. Immune checkpoint inhibitors (ICIs), particularly pembrolizumab—a programmed death-1 (PD-1) receptor blocker—have been integrated with chemotherapy regimens, significantly enhancing anti-tumor efficacy by reactivating the patient’s immune response. Nonetheless, this promising synergy brings complexities related to safety and adverse event management, necessitating comprehensive real-world evaluations beyond controlled clinical trials.
A groundbreaking study utilizing data from the FDA Adverse Event Reporting System (FAERS) has sought to characterize the safety profile and associated risks of combining pembrolizumab with conventional pemetrexed and platinum chemotherapy in lung cancer patients. This post-marketing pharmacovigilance investigation spans from mid-2017 to late 2024, reflecting the adoption curve and clinical utilization trends of pembrolizumab within routine practice. By employing advanced statistical disproportionality methods, including Reporting Odds Ratio (ROR) and the Bayesian Confidence Propagation Neural Network (BCPNN), the research dissects the relative incidence of adverse events, thereby providing valuable insights into the risk-benefit landscape of this combination therapy.
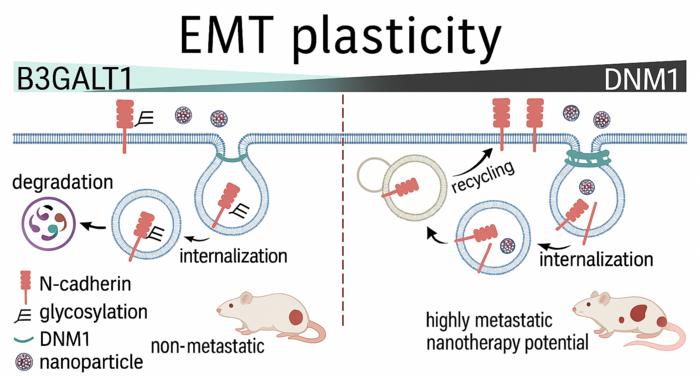
Delving into the FAERS database, the study parsed through thousands of individual adverse event reports: 2,871 instances associated with chemotherapy alone and a considerably larger cohort of 5,443 reports linked to the chemo-immunotherapy combination. This discrepancy not only illustrates the expanding reliance on pembrolizumab-augmented regimens but also foregrounds the imperative to rigorously scrutinize emerging toxicity patterns. The comparative analysis revealed that combination therapy corresponded with heightened frequencies of renal and urinary tract disorders, hepatobiliary complications, and notably, respiratory toxicities such as interstitial lung disease (ILD) and pneumonitis—adverse events that pose clinical management challenges due to their severity and impact on patient quality of life.
Among these findings, the emergence of ILD and pneumonitis as significant risks under the combined therapeutic protocol demands special attention. These pulmonary adverse events are relatively rare yet severe, often requiring early intervention to prevent progression and fatal outcomes. Data indicate the highest susceptibility within the initial three months following treatment initiation, underscoring the necessity for vigilant clinical surveillance during this critical period. The study advocates that oncologists enhance monitoring frameworks and patient education about early respiratory symptoms to promptly address these immune-related toxicities.
Further stratification of data according to patient demographics uncovered meaningful variations in adverse event susceptibility linked to age and gender. Such differential risk patterns highlight the importance of personalized medicine approaches in oncology care. Tailoring patient monitoring and therapeutic dosing on the basis of individual factors could mitigate toxicity rates and improve tolerability, enhancing therapeutic adherence. This discovery stimulates a call for additional research, potentially exploring the genetic, hormonal, or pharmacokinetic bases underlying these subgroup differences, thereby refining patient selection criteria for combination regimens.
Notably, an intriguing aspect of the study is the observed delay in the onset of adverse events when pembrolizumab is added to chemotherapy. While chemotherapy-associated toxicities tend to manifest relatively promptly, the immune-related adverse events elicited by pembrolizumab often present later and may extend over a prolonged clinical course. This temporal divergence emphasizes the need for extended patient follow-up protocols post-combination therapy and informs clinical decision-making regarding monitoring schedules and supportive care measures.
Methodologically, the study stands out by incorporating an array of disproportionality algorithms to interrogate the FAERS data comprehensively. By integrating frequentist tools like the ROR and Proportional Reporting Ratio (PRR) alongside Bayesian models such as the BCPNN and Multi-Item Gamma Poisson Shrinker (MGPS), the researchers achieved a rigorous validation of safety signals. This multi-faceted analytic approach reduces the risk of false-positive findings and strengthens confidence in identifying authentic adverse event associations in the diverse, real-world patient population captured within the FAERS registry.
While randomized controlled trials remain indispensable for establishing initial efficacy and safety signals, this FAERS-based post-marketing evaluation supplements that evidence by revealing the complexity of adverse events in everyday clinical settings. The heterogeneity of patient comorbidities, varying adherence conditions, and broader demographic representation provide a realistic picture of the safety challenges oncologists face. Consequently, these real-world data serve as an essential complement that guides clinicians in balancing the promise of pembrolizumab-enhanced chemotherapy against potential harms.
The clinical implications of these findings are manifold. Oncologists must carefully balance the enhanced survival benefits offered by pembrolizumab combinations with the elevated risks of renal, hepatic, and pulmonary toxicities. Proactive risk stratification, longitudinal patient monitoring, and prompt management of emerging adverse events are critical components of optimizing therapy. Enhanced patient counseling and education on symptom awareness become pivotal, especially for vulnerable populations identified by the study. Furthermore, the insights could inform modifications to clinical protocols or dosing strategies to ameliorate risks without compromising efficacy.
Looking ahead, the study highlights avenues for future research including in-depth mechanistic investigations into why the combination of pembrolizumab with chemotherapy predisposes to specific toxicities. Integrating biomarker discovery into clinical practice might allow for the early identification of patients with heightened susceptibility to adverse events. Such predictive tools could facilitate the customization of immuno-chemotherapy regimens, aligning with the broader goals of precision oncology. These developments could mitigate complications and enhance the therapeutic index of lung cancer management.
The investigation also underscores the pivotal role of pharmacovigilance databases like FAERS in modern oncology. As big data analytics evolve and healthcare systems generate vast volumes of real-world data, the capacity to detect subtle yet clinically significant safety signals in a timely fashion becomes increasingly vital. Continuous surveillance enables healthcare providers and regulators to adapt treatment guidelines dynamically, ensuring patient safety keeps pace with rapid therapeutic innovation.
In conclusion, the integration of pembrolizumab with pemetrexed and platinum-based chemotherapy marks a significant advance in lung cancer treatment but also introduces a challenging safety profile. This extensive FAERS analysis delineates a nuanced and heightened risk spectrum encompassing renal, hepatic, and pulmonary adverse events that require careful clinical management. Personalized medicine, vigilant monitoring, and real-world evidence-driven adjustments emerge as critical strategies to maximize patient benefit while minimizing harm. As immune-oncology therapies continue to evolve, such insights will remain indispensable in refining treatment paradigms and improving outcomes for patients with lung cancer globally.
In the broader context of oncology, these findings reaffirm the importance of harmonizing innovative therapeutic combinations with meticulous safety assessments in real-world settings. Embracing comprehensive pharmacovigilance and integrating patient-specific risk factors can enhance clinicians’ ability to tailor interventions effectively. Through these concerted efforts, the oncology community moves closer to the dual goals of extending survival and preserving quality of life for lung cancer patients facing this formidable disease.
—
Araştırma Konusu: Pemetrexed ve platin bazlı kemoterapi ile pembrolizumab kullanımının akciğer kanseri hastalarındaki güvenlik profili ve advers olay risklerinin FDA Adverse Event Reporting System (FAERS) veritabanı kullanılarak karşılaştırmalı analizi.
Makale Başlığı: The real-world safety profile of pemetrexed and platinum with or without pembrolizumab: insights from a comparative analysis of FAERS database
Web References: https://doi.org/10.1186/s12885-025-14171-3
Doi Referans: https://doi.org/10.1186/s12885-025-14171-3
Resim Credits: Scienmag.com
Anahtar Kelimeler: akciğer kanseri tedavisi, pembrolizumab, pemetrexed, platin bazlı kemoterapi, immün kontrol noktası inhibitörleri, FDA Adverse Event Reporting System, farmakovijilans, immün ilişkili advers olaylar, interstisyel akciğer hastalığı, pnömonit, kombinasyon tedavisi güvenliği, gerçek dünya verileri, kanser immünoterapisi