Now Reading: NKA’da Kemoterapi Sonrası Lenf Nodü Metastazı Tahmini
-
01
NKA’da Kemoterapi Sonrası Lenf Nodü Metastazı Tahmini
NKA’da Kemoterapi Sonrası Lenf Nodü Metastazı Tahmini
**Cutting-Edge Fusion of CT Radiomics and Clinical Biomarkers Advances Prediction of Lymph Node Metastasis in Gastric Cancer**
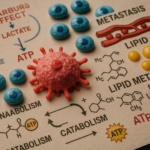
Innovative research has unveiled a transformative approach to predicting lymph node metastasis in patients with locally advanced gastric cancer (LAGC) following neoadjuvant chemotherapy (NAC). By harnessing the power of integrated machine learning models—specifically a stacking classifier that melds radiomic data extracted from computed tomography (CT) with clinical biomarkers—scientists have made a significant leap forward in personalized oncology care. This pioneering fusion technique not only improves diagnostic precision but also promises to optimize treatment strategies, sparing patients from unnecessary interventions and tailoring therapy with unprecedented granularity.
The crux of this study lies in addressing one of oncology’s critical challenges: early identification of lymph node positivity (LN+) after NAC in LAGC, a pivotal factor governing prognosis and subsequent therapeutic decisions. Historically, clinical assessments and imaging techniques posed limitations in sensitivity and specificity, often leading to either overtreatment or undertreatment. Recognizing this gap, researchers embarked on a meticulous process of integrating quantitative imaging features with conventional clinical indicators, applying sophisticated machine learning algorithms to refine predictive accuracy.
Central to the methodology was a retrospective cohort comprising 277 patients diagnosed with LAGC. These individuals underwent pre-treatment portal venous phase CT scans, from which an astounding total of 1,130 radiomic features were extracted. Radiomics, a novel field that converts medical images into high-dimensional, mineable data, captures subtle tumor heterogeneity not discernible by the human eye. This exhaustive feature set formed the raw material for developing a radiomics score (rad score), designed through rigorous feature engineering to distill the most informative imaging biomarkers.
In parallel, a suite of clinical biomarkers—variables known for their prognostic relevance in gastric cancer—were collated. These measures encompassed laboratory values, pathological findings, and demographic data that collectively portray the biological landscape of the tumor and host response. By uniting this clinical data with the synthesized rad score, the researchers sought to construct an overarching predictive framework reflective of both anatomical and biological complexity.
Machine learning played an instrumental role, with the study exploring various statistical approaches to classification. Notably, single ML models, while capable, demonstrated limitations in harnessing the multifaceted data fully. To overcome this, integrated classification strategies were deployed: hard voting, soft voting, and the more sophisticated stacking ensemble method. Stacking, which layers multiple learning algorithms to capitalize on their unique strengths, emerged as the superior strategy—delivering a remarkable area under the receiver operating characteristic curve (AUC) of 0.859 in validation cohorts.
This high AUC underscores an exceptional balance between sensitivity and specificity—critical parameters when predicting LN+, which dictate the intensity and nature of subsequent treatments. The stacking classifier’s enhanced predictive power is attributable to its design that synthesizes divergent model outputs, effectively reducing individual classification bias and variance. This multilevel approach mirrors the complexity of cancer biology and the heterogeneity of patient profiles.
The clinical ramifications of this study are profound. Accurately discerning lymph node metastasis post-NAC equips oncologists with actionable intelligence, enabling more precise risk stratification. Patients with a high likelihood of LN+ might benefit from intensified surveillance or adjunct therapies, while those predicted as lymph node-negative could potentially avoid unnecessary surgical morbidity. More broadly, this methodology paves the way for integrative oncology, wherein data-rich models guide personalized therapy, advancing beyond one-size-fits-all approaches.
Remarkably, the research team has translated their model into a publicly accessible online risk calculator, democratizing access to this cutting-edge tool. This digital resource empowers clinicians globally to input individual patient radiomic scores alongside clinical biomarkers and receive real-time LN+ risk assessments. Such technology-driven decision support facilitates evidence-based clinical judgment, fostering improved outcomes through tailored care pathways.
From a technical standpoint, the rigor of feature selection, model validation, and retrospective design lends robustness to the findings. The training and validation cohorts, split in a 7:3 ratio, ensured that the stacking classifier’s performance was not a product of overfitting but generalizable across diverse patient subsets. Moreover, harmonizing high-dimensional radiomics with tangible clinical markers exemplifies the interdisciplinary synergy between radiology, oncology, and data science.
The implications of this work extend beyond gastric cancer alone. As machine learning increasingly permeates oncologic research, the paradigm exemplified by this study may inspire parallel applications in other malignancies where radiomics and biomarkers interplay critically influences prognosis and treatment decisions. Furthermore, the stacking methodology showcases the potential of ensemble learning to surmount the intricate challenges posed by multi-modal biomedical data.
Nevertheless, certain limitations remain to be addressed in future investigations. The retrospective nature of the study necessitates prospective validation across multi-center populations to ascertain reproducibility and stability under varying clinical contexts. Additionally, integrating genomic data could further enrich the predictive framework, enhancing molecular stratification. Nevertheless, these results represent a significant stride toward fully integrated, precision-driven oncology.
In summary, the fusion of CT radiomics and clinical biomarkers through an integrated machine learning stacking classifier represents a landmark advancement in predicting lymph node metastasis in LAGC patients following NAC. The approach not only exhibits superior predictive performance but also epitomizes the future of personalized cancer care—where computational intelligence unlocks nuanced insights inaccessible to conventional methods. As artificial intelligence continues to evolve, such studies illuminate a path toward more effective, individualized therapeutic regimens that improve survival and quality of life for cancer patients worldwide.
By unlocking the latent data embedded within medical images and marrying them to clinical variables, this research exemplifies the transformative potential of machine learning in healthcare—a beacon for future innovation and clinical impact in oncologic diagnostics and treatment planning.
—
**Subject of Research:**
Prediction of lymph node metastasis in locally advanced gastric cancer integrating CT radiomics and clinical biomarkers through machine learning.
**Article Title:**
Stacking classifiers based on integrated machine learning model: fusion of CT radiomics and clinical biomarkers to predict lymph node metastasis in locally advanced gastric cancer patients after neoadjuvant chemotherapy.
**Article References:**
Ling, T., Zuo, Z., Huang, M. et al. BMC Cancer 25, 834 (2025). https://doi.org/10.1186/s12885-025-14259-w
**Image Credits:**
Scienmag.com
**DOI:**
https://doi.org/10.1186/s12885-025-14259-w
**Keywords:**
clinical biomarkers for gastric cancer, CT radiomics in cancer prediction, fusion of clinical data and imaging, individualized treatment strategies, integrated machine learning models, locally advanced gastric cancer research, lymph node metastasis prediction, machine learning in healthcare, neoadjuvant chemotherapy outcomes, prediction accuracy in oncology, retrospective study on cancer patients, stacking classifiers in machine learning