Now Reading: İnterstisyel Akciğer Hastalıklı Akciğer Kanserli Hastalarda Plevrodezisin Etkinlik ve Güvenlik Değerlendirmesi
-
01
İnterstisyel Akciğer Hastalıklı Akciğer Kanserli Hastalarda Plevrodezisin Etkinlik ve Güvenlik Değerlendirmesi

İnterstisyel Akciğer Hastalıklı Akciğer Kanserli Hastalarda Plevrodezisin Etkinlik ve Güvenlik Değerlendirmesi
Lung cancer and interstitial lung disease (ILD) often coexist, creating complex clinical challenges, especially when malignant pleural effusion (MPE) develops. MPE, the abnormal buildup of fluid in the pleural space caused by tumor invasion or metastasis, significantly worsens respiratory distress and severely undermines patients’ quality of life. Among the most common palliative interventions for MPE is pleurodesis, a procedure designed to obliterate the pleural space by inducing inflammation and fibrosis, effectively preventing recurrent fluid accumulation. However, the presence of ILD—a disease characterized by fragile pulmonary architecture and chronic inflammation—raises important concerns about both the efficacy and safety of pleurodesis in this vulnerable population.
A recently published observational study in the Journal of Thoracic Disease provides valuable insights into this clinical dilemma by evaluating pleurodesis outcomes specifically in lung cancer patients with accompanying ILD. Prior to this research, pleurodesis in such cases was cautiously approached due to the potential for exacerbating lung injury. The study’s contribution lies in its focused analysis of a carefully selected patient cohort, where individuals with partial lung expansion—a known predictor of pleurodesis failure—were excluded. This ensured the evaluation centered on cases where pleurodesis had a realistic potential for success, providing a clearer picture of therapeutic outcomes.
The study reports a pleurodesis efficacy rate of approximately 70% in these patients, a figure comparable to outcomes seen in the general lung cancer population without ILD. This finding challenges the previously held assumption that ILD inherently diminishes pleurodesis success, offering a cautiously optimistic perspective that pleurodesis remains a viable treatment option for symptom management in this complex group. It underscores that, despite the compromised pulmonary milieu in ILD, adequate lung re-expansion and appropriate patient selection can result in meaningful clinical benefits.
Nevertheless, the investigation paints a sobering picture on the safety front. Two patients undergoing pleurodesis developed acute respiratory distress syndrome (ARDS), an alarming and often fatal complication marked by severe lung inflammation and hypoxia. The onset of ARDS post-procedure demands critical attention, especially when weighed against the goal of improving quality of life. This serious adverse event underscores the double-edged nature of pleurodesis in ILD patients, where interventions intended to alleviate symptoms may trigger life-threatening inflammatory cascades.
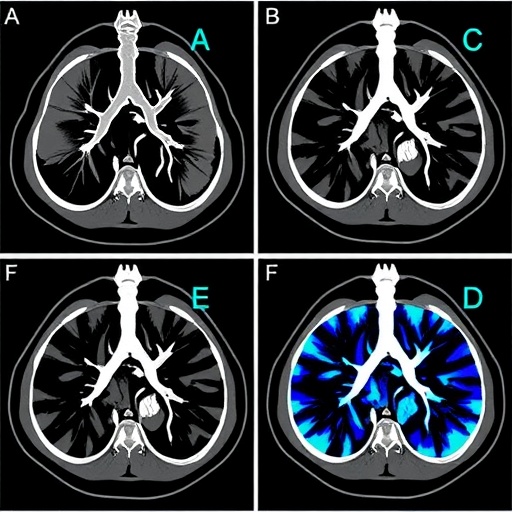
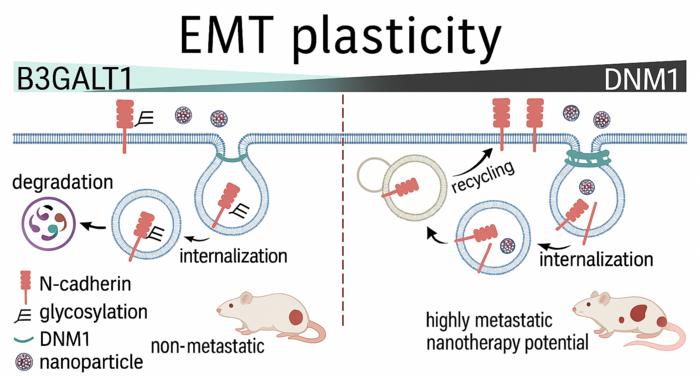
A particularly notable correlation identified in the study is the association between recent systemic prednisolone use for ILD management and the occurrence of ARDS after pleurodesis. Patients who received systemic steroids within six months prior to the procedure and who exhibited radiographic signs such as ground glass opacities and consolidation on imaging were at higher risk for this complication. This suggests that active pulmonary inflammation or immune modulation caused by steroids could predispose these patients to an exaggerated response following pleurodesis-induced inflammation, highlighting the importance of careful clinical assessment of steroid use and ILD activity before proceeding.
Clinicians face a significant challenge in balancing therapeutic benefit against potential harms. Pleurodesis remains a potent palliative tool to ameliorate respiratory discomfort and improve functional status in lung cancer patients with MPE and ILD. Yet, recognizing the risk factors—such as recent steroid therapy and imaging evidence of active pulmonary disease—is crucial for informed decision-making. For high-risk individuals, alternative fluid management strategies may need to be considered, or pleurodesis may require additional precautions and close monitoring during the peri-procedural period.
From a pathophysiological perspective, the study illuminates the fragile equilibrium within the ILD-affected lung microenvironment. The intended inflammation triggered by pleurodesis aimed at sealing the pleural space can inadvertently instigate an overwhelming immune response in already compromised alveolar tissues. Pre-existing inflammatory or fibrotic changes, as signaled by radiographic ground glass opacities, may sensitize the lungs to this provocation, leading to diffuse alveolar damage characteristic of ARDS. This interplay highlights the complexity of inflammation-driven lung injury in ILD patients undergoing invasive interventions.
The choice of sclerosing agent used in pleurodesis also demands consideration. Talc remains the most commonly employed agent due to its effectiveness; however, it has a known association with ARDS, particularly when the talc particle size is not carefully controlled, which can provoke systemic inflammation. Minocycline, an alternative with anti-inflammatory properties, offers promise but requires further study to establish its safety profile in the ILD context. This research utilized both talc and minocycline, yet further randomized controlled trials are necessary to clarify the optimal agent choice to maximize safety and efficacy in patients with coexisting ILD.
This study’s findings argue strongly for the implementation of multidisciplinary care approaches involving oncologists, pulmonologists, and radiologists to optimize treatment planning. Comprehensive pre-procedural evaluation including high-resolution imaging to assess ILD activity, detailed medication history focusing on recent steroid use, and pulmonary function assessment should precede any decision for pleurodesis. Such integrated evaluation facilitates personalized treatment strategies that minimize complications while addressing symptom burdens effectively.
Additionally, this research opens avenues for future investigation into predictive biomarkers that could stratify ARDS risk before pleurodesis. Identification of molecular or inflammatory markers correlated with adverse outcomes could revolutionize patient selection, guiding clinicians toward safer interventions and even prophylactic therapies aimed at mitigating lung injury. Moreover, advances in pleurodesis techniques and exploration of novel sclerosing agents with superior safety profiles could expand options for these fragile patients.
In sum, while pleurodesis emerges from this study as a generally effective palliative measure for lung cancer patients with ILD complicated by MPE, the procedure carries significant risks necessitating circumspect use. The elucidated link between steroid treatment, radiologic disease activity, and ARDS risk underlines the complexity of managing this delicate patient population. Physicians are encouraged to carefully weigh these factors, employ comprehensive assessments, and engage in multidisciplinary collaboration to tailor interventions appropriately.
This pivotal observational study marks a meaningful advance in thoracic oncology and pulmonology by clarifying the nuanced balance between benefit and harm in pleurodesis for ILD-complicated lung cancer. While it fosters hope for symptom relief in a population with limited options, it equally flags the critical need for vigilance, personalized care, and further research. As efforts continue to refine treatment modalities, patient-centered decision-making remains paramount to navigating lung cancer’s challenging intersection with interstitial lung disease.
—
Araştırma Konusu: People
Makale Başlığı: Efficacy and safety of pleurodesis for lung cancer patients with interstitial lung disease
Haberin Yayın Tarihi: 27-Feb-2025
Web References: http://dx.doi.org/10.21037/jtd-24-1541
Doi Referans: 10.21037/jtd-24-1541
Anahtar Kelimeler: Lung cancer, Malignant pleural effusion, Interstitial lung disease, Pleurodesis, Talc, Minocycline, Acute respiratory distress syndrome, Systemic steroids, Pulmonary fibrosis, Thoracic oncology