Now Reading: EGFR Mutasyonlu Akciğer Kanserinde İlk Sırada Osimertinib mi, Sıralı Tedavi mi?
-
01
EGFR Mutasyonlu Akciğer Kanserinde İlk Sırada Osimertinib mi, Sıralı Tedavi mi?

EGFR Mutasyonlu Akciğer Kanserinde İlk Sırada Osimertinib mi, Sıralı Tedavi mi?
Epidermal growth factor receptor (EGFR) mutations play a pivotal role in guiding treatment strategies for non-small cell lung cancer (NSCLC), influencing outcomes significantly across global patient populations. Notably, these activating mutations occur in approximately half of Asian patients diagnosed with NSCLC, while their presence is more limited in Caucasian patients at around 15%. The recognition of these molecular drivers has catalyzed a paradigm shift in therapeutic approaches, elevating tyrosine kinase inhibitors (TKIs) to frontline treatment status. The evolution from first-generation agents like erlotinib and gefitinib to later generations has shaped contemporary standards through landmark clinical trials, yet the optimal sequencing and strategy remain subjects of ongoing investigation.
First-generation EGFR TKIs initially demonstrated substantial clinical benefits, offering targeted therapy options that improved efficacy and tolerability compared with traditional chemotherapy. Trials such as EURTAC and IPASS firmly established erlotinib and gefitinib as viable first-line options for patients harboring sensitizing EGFR mutations. Despite these advances, resistance invariably develops, most commonly through the acquisition of the T790M mutation in exon 20, prompting the need for successive lines of therapy to overcome disease progression.
The advent of osimertinib, a third-generation, irreversible EGFR TKI now firmly entrenched in clinical practice, marked a breakthrough for both frontline and resistance-associated treatment landscapes. The FLAURA trial, a pivotal phase III study, illustrated the superiority of upfront osimertinib compared to first-generation TKIs, demonstrating significant improvements in progression-free and overall survival, alongside enhanced central nervous system (CNS) penetration and tolerability. Nonetheless, an ongoing debate concerns whether initiating therapy with osimertinib or following a sequential approach—starting with first-generation TKIs and moving to osimertinib upon progression—yields better long-term outcomes.
Challenges in interpreting FLAURA’s overall survival data stem partly from limited availability of osimertinib post-progression in the first-generation TKI arms, with only 37.2% of patients receiving osimertinib after failing initial therapy. This limitation potentially amplifies the apparent benefit of upfront osimertinib. In contrast, the APPLE trial, a recent phase II study designed to elucidate sequencing strategies, demonstrated that 73% of patients randomized to gefitinib or erlotinib subsequently crossed over to osimertinib upon progression. This substantial crossover rate offers a more rigorous comparison of treatment strategies within EGFR-mutated NSCLC.
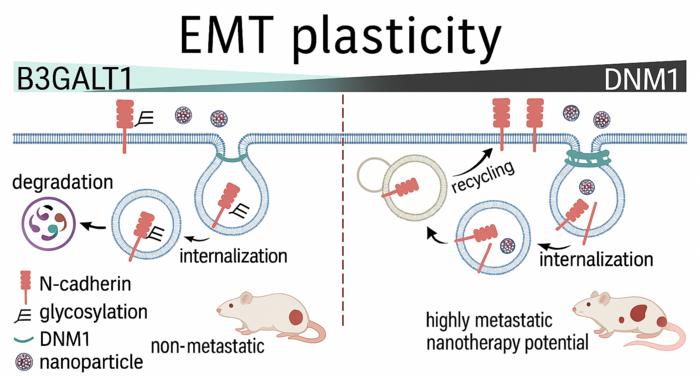
The APPLE trial enrolled treatment-naïve patients harboring the two most common EGFR mutations—exon 19 deletions and L858R—protecting the homogeneity critical for assessing nuanced treatment effects. Patients were randomized to three arms: upfront osimertinib (arm A), gefitinib with molecularly guided early switch to osimertinib upon plasma detection of T790M (arm B), and gefitinib with switch to osimertinib at clinical progression by imaging criteria (arm C). This design uniquely interrogated the timing and molecular triggers for transitioning therapies, with the primary endpoint focusing on progression-free survival (PFS) on osimertinib in the molecular-switch arm.
Interestingly, the initial outcomes from APPLE showed that ctDNA-guided early transition to osimertinib did not confer a significant overall survival advantage over conventional clinical progression-based switching. This finding tempered enthusiasm for molecular trigger-based sequencing, especially as osimertinib rapidly became the recommended upfront therapy following FLAURA results. However, recent detailed analyses pooling sequential arms B and C and comparing them against upfront osimertinib (arm A) have resurfaced crucial insights, revealing no significant differences in overall survival between sequential and upfront approaches, particularly in the context of high osimertinib availability post-progression.
The absence of statistically significant survival differences in the APPLE post hoc analysis supports the notion that sequential therapy could remain a viable strategy, especially in regions where upfront osimertinib access is limited by cost or regulatory restrictions. Yet, caution is warranted given the study’s phase II, non-comparative design and modest patient numbers, which limit definitive conclusions. Moreover, the aggregation of two distinct sequential arms into one analytical group introduces potential biases due to differences in patient characteristics and timing of molecular monitoring.
From a practical standpoint, the sequential approach hinges heavily on the reliable detection of the T790M resistance mutation, which affords patients eligibility for second-line osimertinib. This requirement introduces complexities, including the risk of patients not developing the mutation, inadequate access to molecular testing because of financial or infrastructural limitations, or clinical deterioration precluding subsequent therapy. While only a small fraction (around 4%) of APPLE participants were unable to receive second-line treatment, real-world rates might be substantially higher, potentially diminishing the sequential strategy’s applicability.
Safety profiles emerged as an additional advantage for sequential therapy, with second-line osimertinib demonstrating excellent tolerability and reduced incidences of dermatologic toxicities commonly associated with first-generation TKIs. This enhanced tolerability could translate into better patient quality of life during salvage therapy. Furthermore, there may be specific patient subgroups—such as those experiencing central nervous system progression—who could derive particular benefit from second-line osimertinib, given its superior CNS penetration and activity.
Central nervous system disease control remains a critical consideration in choosing treatment sequences. The APPLE trial revealed that median brain progression-free survival was markedly longer with upfront osimertinib compared to sequential therapy, underscoring osimertinib’s ability to delay intracranial metastases. Despite imbalances in baseline brain metastasis prevalence favoring the sequential arm, the data validate guidelines recommending osimertinib for patients with CNS involvement at diagnosis. Nevertheless, ongoing trials like FLAURA2 and MARIPOSA, which explore combinations of osimertinib with chemotherapy or novel agents such as amivantamab and lazertinib, continue to evolve clinical options and complicate decision-making regarding optimal upfront regimens for this vulnerable subgroup.
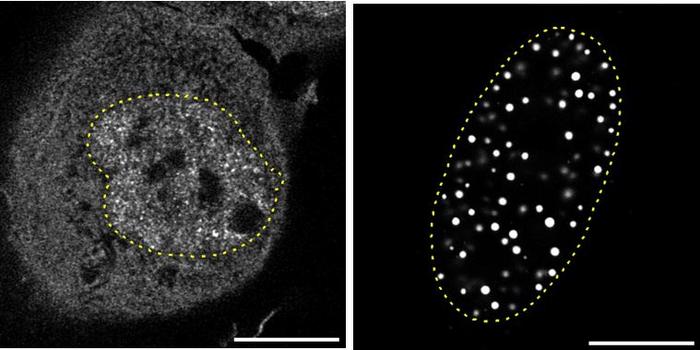
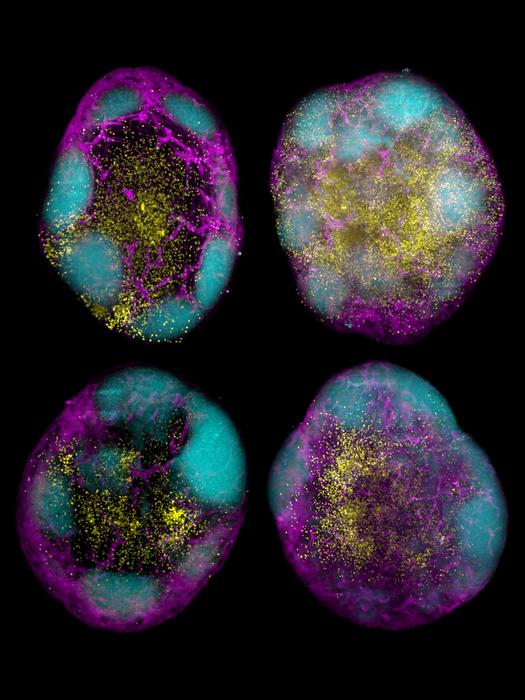
A promising frontier in therapy optimization is the integration of circulating tumor DNA (ctDNA) dynamics into clinical algorithms. The APPLE trial demonstrated the feasibility of serial plasma monitoring using the Cobas EGFR test to detect T790M emergence, highlighting the potential of liquid biopsies to guide treatment transitions. Furthermore, accumulating evidence links ctDNA clearance following therapy initiation to improved progression-free survival, as shown in multiple studies including the FLAURA, AURA3, and MARIPOSA trials.
Despite these advances, translation of ctDNA into a clinically validated, dynamic biomarker for routine decision-making requires overcoming technical, logistical, and economic hurdles. Assay sensitivities vary considerably: the Cobas PCR assay used in APPLE is less sensitive than droplet digital PCR or next-generation sequencing methods employed in other trials, which also detect a broader spectrum of resistance mutations beyond T790M. Whether higher sensitivity assays can sharpen prognostic correlations or therapeutic guidance remains an important open question.
Cost considerations loom large, particularly in resource-constrained settings, since more sensitive assays are often more expensive and frequent serial sampling may not be practical. Designing prospective, randomized trials to robustly establish the impact of ctDNA-guided treatment modifications is inherently complex but essential for defining evidence-based clinical pathways.
Looking forward, the rapid evolution of treatment paradigms, with intensified upfront regimens and combination therapies under investigation, accentuates the pressing need for predictive biomarkers that can discriminate between patients best suited for upfront osimertinib versus those who may benefit from a sequenced approach. The absence of such tools currently limits personalized treatment selection, increasing reliance on clinical factors and drug access considerations.
In summary, the emerging data from the APPLE trial enrich our understanding of frontline and sequential TKI strategies in EGFR-mutant NSCLC, suggesting that while upfront osimertinib remains a standard of care due to superior CNS control and proven survival benefits, sequential approaches retain relevance, especially where resource constraints exist. The prognostic utility of ctDNA monitoring offers an exciting avenue toward individualized therapy adjustments, although further validation is required before widespread clinical adoption. Ultimately, the ongoing expansion of therapeutic options calls for integrative biomarkers and smart sequencing decisions, navigating a complex landscape to optimize long-term patient outcomes.
—
Araştırma Konusu: EGFR mutasyonlu metastatik küçük hücre dışı akciğer kanserinde osimertinib öncelikli ve sekans tedavi stratejilerinin karşılaştırılması, beyin metastazlarının kontrolü ve dolaşımdaki tümör DNA’sının (ctDNA) tedavi yanıtı ile ilişkisi.
Makale Başlığı: The APPLE’s core question—upfront osimertinib versus the sequential approach for EGFR mutated non-small cell lung cancer
Haberin Yayın Tarihi: 25 Şubat 2025
Web References:
– https://doi.org/10.21037/jtd-24-1785
– Ramalingam SS et al. N Engl J Med 2020;382:41-50 (FLAURA trial)
– Remon J et al. Ann Oncol 2023;34:468-76 (APPLE trial initial publication)
– Remon J et al. J Clin Oncol 2024;42:1350-6 (APPLE trial update)
Doi Referans: 10.21037/jtd-24-1785
Anahtar Kelimeler: EGFR mutations in lung cancer, non-small cell lung cancer, osimertinib, tyrosine kinase inhibitors, APPLE trial, FLAURA trial, sequencing strategies, T790M resistance mutation, circulating tumor DNA, progression-free survival, brain metastasis control, targeted therapy