Now Reading: Çinli Multipl Miyelom Hastalarında Daratumumab Analizi
-
01
Çinli Multipl Miyelom Hastalarında Daratumumab Analizi
Çinli Multipl Miyelom Hastalarında Daratumumab Analizi
A groundbreaking observational study emerging from China has now shed new light on how daratumumab, a monoclonal antibody directed against CD38, is being integrated into treatment regimens for multiple myeloma (MM) patients in a real-world clinical setting. While the efficacy of daratumumab-based therapies has been well-documented through randomized controlled trials globally, this extensive analysis of Chinese patients affirms its clinical utility, highlighting real-world treatment patterns, safety profiles, and patient outcomes, thereby providing invaluable data to bridge clinical trials and everyday practice.
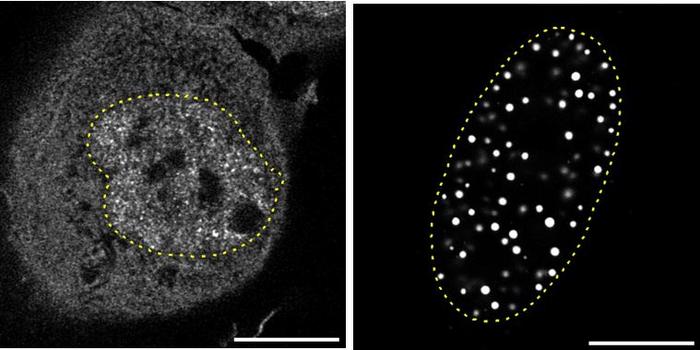
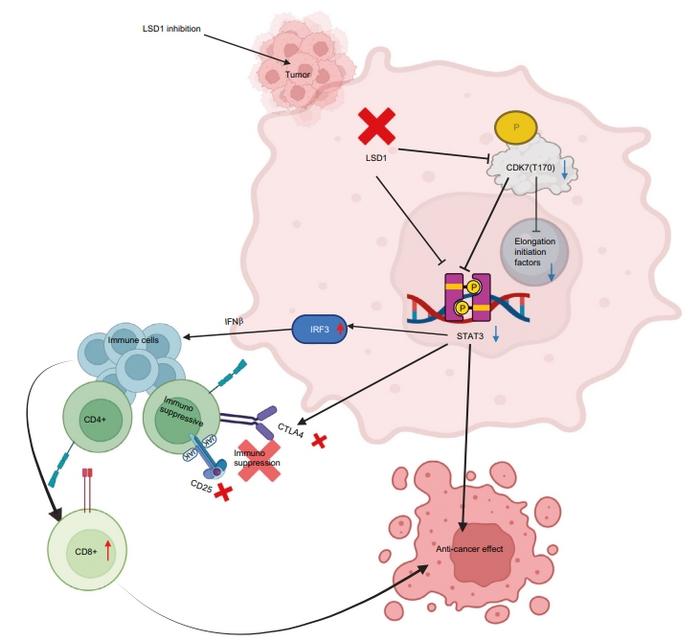
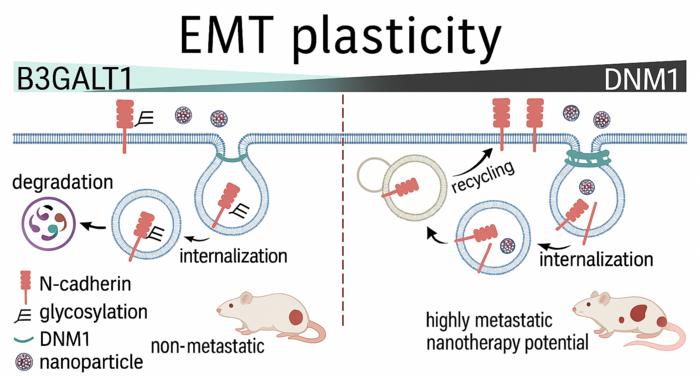
Daratumumab’s mechanism of action is multifaceted, targeting the CD38 antigen—which is abundantly expressed on myeloma cells—not only to induce direct tumor cell death but also to modulate the immune environment. This dual approach disrupts tumor progression and reactivates immune surveillance, representing a significant advance in MM therapy. The drug’s incorporation into various backbone regimens reflects an evolving landscape of combinational strategies optimized to enhance response rates while managing toxicity.
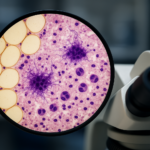
This large-scale observational study enrolled 212 patients across 13 medical centers in China, including both newly diagnosed and relapsed/refractory MM cases. The patient cohort was carefully selected to reflect real-world complexity, with individuals having received up to three prior lines of treatment, ensuring that findings pertain to early and intermediate disease scenarios. Data collection was both prospective and retrospective, allowing comprehensive insight into daratumumab’s utility in routine clinical workflows.
Treatment regimens varied widely, encompassing daratumumab monotherapy, its combination with dexamethasone alone, combinations with proteasome inhibitors (PIs) either with or without dexamethasone, immunomodulatory drugs (IMiDs) with or without dexamethasone, and multi-agent regimens combining PIs and IMiDs. The diversity of regimens underlines physicians’ flexibility in tailoring therapy to patient needs and the growing acceptance of daratumumab-based protocols across treatment lines.
Remarkably, daratumumab was initiated at different points in the treatment chronology: 16.5% of patients commenced daratumumab in the frontline setting, over half in the second line, with remaining patients starting in later lines. This spread reflects the adaptation of daratumumab beyond initial diagnosis into the relapsed and refractory space, showcasing its versatility and relevance across disease stages.
Efficacy analyses revealed encouraging response rates, with nearly three-quarters of patients achieving at least a partial response. More than half experienced a very good partial response or better, outcomes that align with—but crucially validate beyond controlled trials—previous evidence attesting to daratumumab’s robust anti-myeloma activity. These data were further reinforced by progression-free survival metrics, where estimated 6- and 12-month rates highlighted a sustained disease control achievable with daratumumab regimens.
Efficacy was notably superior in combination therapies compared to daratumumab monotherapy, suggesting that the synergy between daratumumab and other agents such as PIs and IMiDs meaningfully enhances therapeutic impact. This finding supports ongoing clinical strategies favoring combinational approaches and signals promising pathways for improving patient prognoses.
Safety profiles in this real-world cohort were consistent with known adverse event patterns of daratumumab. Approximately 13.7% of patients experienced serious treatment-emergent adverse events, with pneumonia emerging as the most common serious complication, occurring in 4.7% of patients. Hematologic toxicities such as leukopenia, neutropenia, and thrombocytopenia were the most common adverse drug reactions reported, underscoring the importance of vigilant hematologic monitoring during therapy.
The study’s extensive observational design enhances the significance of the safety data, reflecting a more heterogeneous patient population than typical clinical trials. This real-life context is invaluable for clinicians contemplating daratumumab for diverse patients, including those with comorbidities and varying degrees of prior treatment exposure.
Importantly, the continued collection of follow-up data from this patient cohort promises to refine our understanding of long-term outcomes, resistance patterns, and the longitudinal safety of daratumumab-containing regimens in routine care. These ongoing insights will augment current knowledge and potentially inform updated treatment algorithms tailored for Chinese patient populations.
This research is emblematic of the broader trend towards integrating real-world evidence into oncology, juxtaposing controlled trial data with pragmatic, patient-centered outcomes. It uniquely captures treatment dynamics within China, a key player in global oncology, thereby extending the global evidence base and providing region-specific perspectives essential for personalized medicine.
Moreover, this study underscores the critical role monoclonal antibodies play in revolutionizing multiple myeloma treatment paradigms. Daratumumab targeting CD38 illustrates how precision immunotherapy can transform prognosis, extending beyond tumor kill to modulate host immunity, a paradigm now increasingly adopted for hematologic malignancies.
As multiple myeloma remains incurable and prone to relapse, the evolution of therapeutic options is crucial. Daratumumab’s demonstrated efficacy, safety, and adaptability highlighted through this detailed analysis affirm its position as a cornerstone for frontline and salvage therapy, especially when combined thoughtfully with proteasome inhibitors and immunomodulatory agents.
Ultimately, the integration of real-world data such as these enriches clinical decision-making, harnessing global evidence while respecting regional treatment realities. For patients battling multiple myeloma across China, this study offers optimism and a clearer roadmap for personalized, effective, and tolerable treatment regimens centered on daratumumab’s unique therapeutic profile.
In conclusion, this comprehensive real-world study establishes daratumumab-based therapy as a proven and safe cornerstone in managing both newly diagnosed and relapsed/refractory multiple myeloma among Chinese patients. Continued research and data collection will no doubt further elucidate how best to deploy these regimens to maximize patient benefit and improve survival outcomes in clinical practice across varied healthcare settings worldwide.
—
**Subject of Research:**
Real-world treatment patterns, effectiveness, and safety of daratumumab-based regimens in multiple myeloma patients in China
**Article Title:**
Real-world analysis of treatment patterns, effectiveness, and safety of daratumumab-based regimens in Chinese patients with newly diagnosed or relapsed/refractory multiple myeloma
**Article References:**
Wang, L., Yang, W., Wang, Y. et al. BMC Cancer 25, 836 (2025). https://doi.org/10.1186/s12885-025-13925-3
**DOI:**
https://doi.org/10.1186/s12885-025-13925-3
**Image Credits:**
Scienmag.com
**Keywords:**
CD38 targeting in multiple myeloma, clinical daratumumab treatment patterns in China, effectiveness of daratumumab in multiple myeloma, immunomodulatory effects of daratumumab, monoclonal antibodies in cancer therapy, newly diagnosed multiple myeloma in Chinese patients, observational study on daratumumab, real-world analysis of multiple myeloma treatment, relapsed refractory multiple myeloma treatment options, safety of daratumumab regimens, standard care for multiple myeloma