Now Reading: Karbolplatinin TNBC’deki HER2 Düzeylerine Etkisi
-
01
Karbolplatinin TNBC’deki HER2 Düzeylerine Etkisi
Karbolplatinin TNBC’deki HER2 Düzeylerine Etkisi
In recent years, the landscape of treatment for triple-negative breast cancer (TNBC) has been one of the most challenging frontiers in oncology due to the aggressive nature of this disease and the lack of targeted therapies. A newly published multicenter real-world analysis sheds important light on the role of carboplatin, a platinum-based chemotherapy agent, in enhancing treatment responses in TNBC patients receiving neoadjuvant chemotherapy. This groundbreaking investigation specifically delves into how the efficacy of carboplatin varies based on nuanced HER2 expression profiles, categorized as HER2-low and HER2-zero status, providing crucial insights that may influence future therapeutic strategies.
TNBC, defined by its lack of estrogen receptor (ER), progesterone receptor (PR), and HER2 overexpression, frequently portends a worse prognosis compared to other breast cancer subtypes due to its rapid progression and limited targeted options. Neoadjuvant chemotherapy (NACT) remains a cornerstone in managing locally advanced TNBC, aiming to reduce tumor burden preoperatively and provide an early indication of chemotherapy response. However, heterogeneity within TNBC subgroups, particularly in terms of HER2 expression levels, has raised critical questions about how best to tailor chemotherapy regimens to maximize patient outcomes.
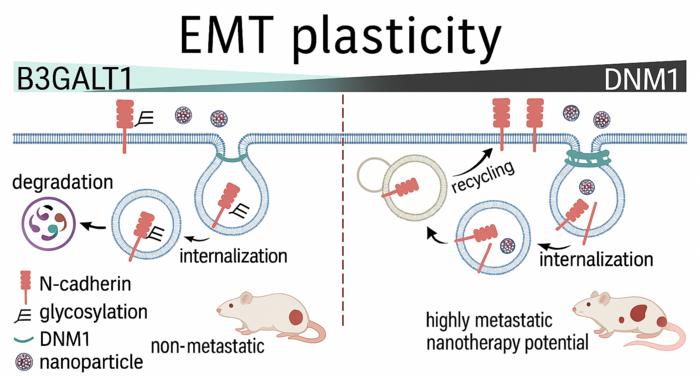
This extensive study gathered data from 269 patients treated across five oncology clinics, stratifying participants by their HER2 expression status into two groups: HER2-low (56.5%) and HER2-zero (43.5%). This binary classification is particularly relevant as emerging evidence suggests that HER2-low breast cancers may represent a biologically and clinically distinct entity from tumors entirely devoid of HER2 expression. Such differentiation could influence therapeutic decision-making, especially concerning the introduction of agents like carboplatin, known for its DNA-damaging effects.
The analysis revealed a striking difference in pathological complete response (pCR) rates between the two HER2 cohorts. Patients categorized as HER2-zero demonstrated significantly higher pCR rates compared to their HER2-low counterparts, with figures of 45.2% versus 23.7% respectively. This finding is notable because achieving pCR following neoadjuvant chemotherapy is strongly correlated with improved prognosis and longer survival in breast cancer. Understanding the biological underpinnings of this disparity could be pivotal in optimizing treatment regimens tailored to HER2 expression levels.
When carboplatin was added to the neoadjuvant chemotherapy protocol, both groups benefited from enhanced pCR rates, but the effect was more pronounced in the HER2-zero subgroup. In this group, carboplatin administration elevated pCR rates dramatically to 63.3%, compared to 39.0% in patients who did not receive the drug. HER2-low patients also experienced a significant improvement, with pCR rates rising to 36.8% from 19.3%. This data robustly supports the addition of carboplatin to standard chemotherapy in TNBC patients regardless of HER2 status, emphasizing a paradigm shift towards more personalized chemotherapy regimens.
Intriguingly, the therapeutic benefit of carboplatin was attenuated in specific subpopulations. Patients with Grade 1 tumors—a classification often associated with less aggressive behavior—did not show improved pCR rates with carboplatin, indicating that tumor grade remains a critical factor in predicting chemotherapy responsiveness. Furthermore, HER2 score 2-FISH negative tumors did not experience significant benefits, which underscores the complexity of HER2 biology and suggests that not all HER2-low tumors are equivalent in their treatment sensitivities.
The study also explored whether BRCA mutation status, a known predictor of platinum sensitivity due to defects in DNA repair mechanisms, modified the benefit obtained from carboplatin. Surprisingly, no statistically significant difference was observed, suggesting that carboplatin’s impact transcends BRCA mutation status and may be universally advantageous in TNBC settings. This finding challenges prior assumptions and raises questions about the mechanisms by which carboplatin enhances tumor eradication in TNBC beyond classical homologous recombination deficiency alone.
Survival analyses further solidified the clinical importance of achieving pathological complete response. Patients who attained pCR exhibited significantly prolonged disease-free survival (DFS) and overall survival (OS), emphasizing pCR as a meaningful surrogate endpoint in neoadjuvant trials. The data reinforced that carboplatin-enhanced pCR rates ultimately translate into durable clinical benefit, affirming the drug’s role in improving long-term outcomes for TNBC patients.
This study’s multicenter real-world design adds valuable external validity to its findings. While randomized controlled trials remain the gold standard for clinical evidence, real-world data from diverse clinical settings often reveal nuances reflecting everyday treatment challenges and patient heterogeneity. The consistency of carboplatin’s benefit across various centers and subpopulations strengthens the argument for its routine consideration in appropriate TNBC neoadjuvant protocols.
However, the study also acknowledges that carboplatin is not without its toxicities. Myelosuppression, nephrotoxicity, and neurotoxicity are well-known adverse effects that necessitate careful patient selection and vigilant monitoring. The authors prudently recommend integrating carboplatin into treatment only after assessing individual patient factors, including performance status and comorbidities, to optimize the therapeutic index.
Incorporating carboplatin into the therapeutic landscape of TNBC aligns with the broader movement towards precision oncology, where molecular and histopathological tumor characteristics guide tailored treatment approaches. This research contributes important data suggesting that HER2-low versus HER2-zero status, traditionally underrecognized in TNBC management, may serve as a biomarker for informing chemotherapy intensification strategies.
The implications of these findings extend beyond immediate treatment choices, potentially influencing clinical trial designs focused on TNBC. Future studies might explore combinations of carboplatin with emerging agents, immunotherapy, or targeted therapies specific to HER2-low tumors. Additionally, mechanistic studies to unravel why HER2-zero tumors respond better to platinum agents could unveil novel therapeutic targets.
Notably, the research highlights that triple-negative breast cancer remains a heterogeneous disease entity, requiring nuanced approaches rather than one-size-fits-all therapies. Validating the delineation of HER2-low and HER2-zero tumors distinctively in clinical practice will be critical. The findings prompt a reevaluation of current diagnostic algorithms and encourage a more granular pathology assessment to inform treatment planning.
In conclusion, this comprehensive multicenter analysis elucidates the positive impact of carboplatin in boosting pathological complete response rates across HER2-low and HER2-zero TNBC subgroups and underscores the predictive value of pCR for survival outcomes. As carboplatin-containing regimens become increasingly integrated into neoadjuvant protocols, oncologists are equipped with more robust evidence to optimize patient management and improve prognoses in one of the most aggressive breast cancer subtypes.
This study marks a significant advance in the ongoing quest to refine and personalize treatment for triple-negative breast cancer. The data compellingly advocate for incorporating carboplatin into neoadjuvant chemotherapy regimens for eligible patients, irrespective of HER2 expression nuances, with the caveat of weighing individual patient factors and toxicity profiles. Future research inspired by these findings will undoubtedly continue to unravel the complexities of TNBC and propel progress in this critical area of oncology.
—
**Subject of Research:** The efficacy of carboplatin addition to neoadjuvant chemotherapy in triple-negative breast cancer patients stratified by HER2-low and HER2-zero status.
**Article Title:** The impact of carboplatin on pathologic complete response and survival based on HER2 low and HER2 zero status in triple negative breast cancer patients receiving neoadjuvant chemotherapy: a multicenter real-world analysis.
**Article References:**
Yıldırım, S., Başoğlu, T., Doğan, A. et al. BMC Cancer 25, 833 (2025). https://doi.org/10.1186/s12885-025-14252-3
**Image Credits:** Scienmag.com
**DOI:** https://doi.org/10.1186/s12885-025-14252-3
**Keywords:** carboplatin treatment in triple negative breast cancer, chemotherapy response in HER2 subgroups, efficacy of carboplatin in chemotherapy, HER2 zero status in triple negative breast cancer, impact of carboplatin on survival rates, multicenter analysis of cancer treatment, neoadjuvant chemotherapy for HER2 low status, neoadjuvant therapy effectiveness in TNBC, pathologic complete response in TNBC, real-world study on breast cancer, survival outcomes in breast cancer patients, triple-negative breast cancer prognosis