Now Reading: Grade 2 Meningiomlarda Gamma Knife Radyocerrahinin Yönetimdeki Rolü
-
01
Grade 2 Meningiomlarda Gamma Knife Radyocerrahinin Yönetimdeki Rolü
Grade 2 Meningiomlarda Gamma Knife Radyocerrahinin Yönetimdeki Rolü
The management of grade 2 meningiomas has long posed significant challenges for neurosurgeons and oncologists, primarily due to the aggressive nature and recurrence potential of these intermediate-grade tumors. As conventional treatment modalities evolve, stereotactic radiosurgery, particularly Gamma Knife Radiosurgery (GKRS), has attracted considerable attention for its precision and minimally invasive approach. A recent comprehensive study sheds light on the long-term efficacy and outcomes of GKRS in treating grade 2 meningiomas, offering crucial insights into tumor control, dosimetry considerations, and survival rates.
Grade 2 meningiomas occupy a grey zone between benign and highly malignant intracranial tumors, characterized by increased mitotic activity and a propensity for recurrence. Surgical resection remains the frontline treatment; however, complete excision is often unachievable without risking neurological deficits due to tumor location. GKRS, employing focused gamma radiation beams, emerges as a promising adjuvant or primary treatment alternative that offers localized tumor irradiation with minimal damage to adjacent healthy tissue.
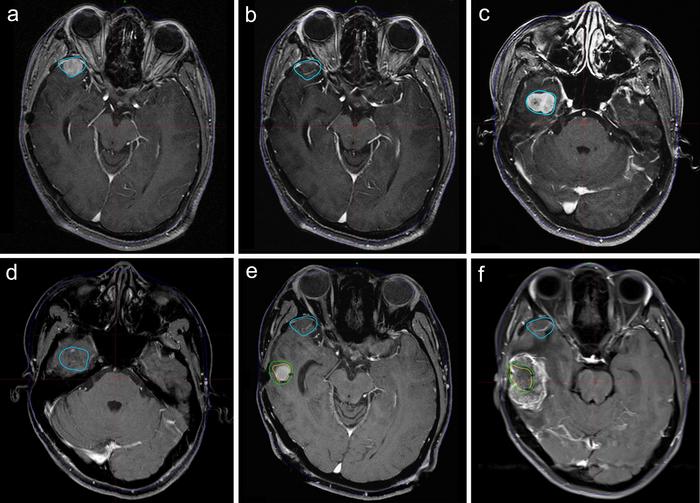
Over a nearly decade-long retrospective analysis encompassing seventy patients treated between 2007 and 2016, researchers utilized GKRS to target grade 2 meningiomas and meticulously evaluated treatment outcomes. The median follow-up period of 48 months provided a substantial temporal window to assess progression-free survival, local tumor control, and potential adverse effects stemming from radiosurgical intervention. This extent of follow-up surpasses many prior studies, furnishing robust data on long-term efficacy.
The study revealed a one-year local tumor control rate of 92%, which decreased to 73% at three years and further to 65% by five years post-GKRS. While initial response rates appear promising, these statistics underscore the recurrent nature of grade 2 meningiomas and highlight the limitations of radiosurgery as a definitive monotherapy. The corresponding progression-free survival rates at one, three, and five years were 87%, 51%, and 44%, respectively, reflecting the ongoing risk of tumor progression despite targeted treatment.
One of the paramount findings from this cohort is the impact of multiple lesions and previous recurrence episodes on treatment outcomes. Patients harboring multiple meningiomas or those who had experienced several prior recurrences demonstrated significantly diminished rates of marginal tumor control and progression-free survival. These factors evidently act as negative prognostic indicators, suggesting that such patients may require more aggressive or combinatorial treatment strategies beyond GKRS alone.
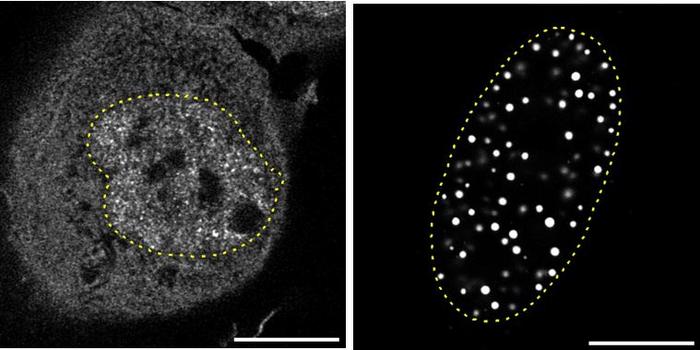
Dosimetry, or the calibration of radiation dose delivered to the target tumor margins, emerged as another critical determinant of treatment success. Marginal doses of 13 Gy or less were significantly associated with poorer local tumor control. This observation advocates for the administration of higher prescription doses to optimize tumor eradication while balancing the risk of radiation-induced toxicity. Precision in isodose line targeting—the specific radiation dose contour enveloping the tumor—is vital in achieving maximal effect.
The study also chronicled the clinical course of patients who underwent multiple rounds of GKRS for newly developed meningiomas. In one highlighted case, an initial 12 Gy dose at a 50% isodose line resulted in significant tumor shrinkage at the six-month follow-up. Subsequent tumors were treated with escalating prescription doses—14 Gy at 52% and 13 Gy at 50% isodose lines—with varying degrees of tumor response documented at extended follow-ups. This case exemplifies the dynamic nature of tumor progression post-radiosurgery and the necessity for vigilant longitudinal monitoring.
Despite certain patients requiring repeated intervention, overall serious complications directly attributed to GKRS were relatively rare, with only 4% experiencing significant adverse events. This relatively favorable safety profile strengthens the argument for GKRS as a viable, minimally invasive modality even in the setting of recurrent disease. Nonetheless, the balance between dose intensification and toxicity risk remains a pivotal consideration in treatment planning.
An additional noteworthy aspect detailed by the researchers concerns outfield progression—recurrences occurring outside the originally targeted margins. This phenomenon was notably prevalent among patients with high-risk features such as multiple prior recurrences and multifocal disease. The findings suggest that while GKRS achieves commendable local control within the treated volume, its reach in preventing distant tumor evolution is limited, prompting interest in integrated therapeutic approaches.
The practical implications extend beyond the sphere of neurosurgery, emphasizing the need for a multidisciplinary approach encompassing neuro-oncology, radiation oncology, and imaging specialists. Optimization of follow-up imaging schedules and dose adjustments tailored to individual risk profiles may enhance long-term outcomes. Furthermore, adjunctive external beam radiotherapy (EBRT) or novel systemic therapies could synergistically augment GKRS efficacy in complex cases.
Ultimately, this landmark study supports the considered use of GKRS in managing grade 2 meningiomas, particularly where surgical options are constrained. It also spotlights the necessity of personalized treatment regimens, higher margin doses, and comprehensive surveillance to mitigate the inherent challenges posed by these tumors. As the field continues to evolve, ongoing research into radiosurgical innovations and combined modality treatments will be crucial in refining outcomes.
Gamma Knife Radiosurgery represents a transformative tool in the neurosurgical armamentarium, marrying technological precision with clinical practicality. Its role in the nuanced landscape of grade 2 meningioma management exemplifies the intersection of modern radiation physics, neuro-oncology, and patient-centric care. This comprehensive evaluation sets the stage for future prospective trials aiming to validate optimized protocols and integrate systemic therapies alongside GKRS.
The long-term survival and control rates documented in this study establish a benchmark, confirming GKRS as a reasonable and effective treatment avenue. However, acknowledging the biological aggressiveness of grade 2 meningiomas and their recurrence profile, more aggressive or multimodal therapeutic strategies may be necessary for patients exhibiting unfavorable risk factors. As research progresses, the personalized application of GKRS, informed by lesion characteristics and prior treatment history, promises to enhance patient outcomes further.
In sum, the nuanced understanding of radiosurgical dose-response relationships, tumor biology, and recurrence patterns offered by this investigation enriches the clinical decision-making process. Weighting the benefits of tumor control against potential risks and incorporating patient-specific factors will be paramount in optimizing care pathways for individuals diagnosed with grade 2 meningiomas.
—
**Subject of Research**: The long-term outcomes and efficacy of Gamma Knife Radiosurgery in the treatment of grade 2 meningiomas
**Article Title**: The Role of Gamma Knife Radiosurgery in the Management of Grade 2 Meningioma
**News Publication Date**: 17-Dec-2024
**Web References**: Not provided
**Doi Referans**: 10.14218/NSSS.2024.00002
**Resim Credits**: Shibin Sun, Enmeng Bao
**Anahtar Kelimeler**: case studies in gamma knife radiosurgery, effectiveness of gamma knife in tumor control, external beam radiotherapy vs GKRS, follow-up results of gamma knife treatment, gamma knife radiosurgery for meningioma, isodose line in GKRS treatment, long-term outcomes of meningioma treatment, management of grade 2 meningioma, new tumor development post-radiosurgery, precision in radiosurgery dosing, prescription dose in radiosurgery, tumor shrinkage after GKRS